By Caleb Takyi
What is Narcolepsy?
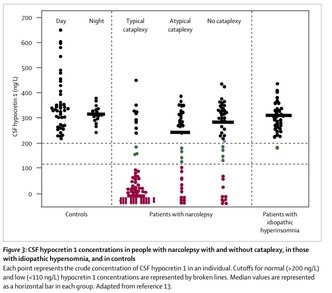
Over the past few decades, advancements in research have to new ways of understanding the chemistry of the brain. One such way is collecting cerebrospinal fluid and measuring the amount of hypocretin molecules present in the fluid. In the study conducted by Mignot, patients had some cerebrospinal fluid drawn and examined while the underwent a multiple sleep latency test (MLST). This MLST is an assessment of how quickly one falls asleep in a quiet environment. This revealed that the lack of hypocretin has been linked to narcolepsy. Below is a chart depicting hypocretin levels in a patient with narcolepsy with or without cataplexy. Cataplexy is a disease commonly associated with Narcolepsy. This disease causes muscle weakness, further explanation will be in the next section. It also compares the hypocretin levels to a normal brain and an idiopathic hypersomniac (Figure 3).
narcolepsy image 1The possible cause is the destruction of hypocretin-producing cells located in the hypothalamus (Lee & Radin 1). According to Lee and Radin, narcolepsy is estimated to affect 25 to 50 per 100,000 people (1). Even without cataplexy (episodes of muscle weakness), narcolepsy alone can prove to be a very challenging disease for the sizable number of sufferers. Although narcolepsy is due to a lack of hypocretin, not much is known about what destroys these hypocretin-producing cells. There is evidence arising that it is an autoimmune disorder. Autoimmune disorders are caused when the immune system mistakenly attacks healthy tissues and cells in the body. For narcolepsy, the immune system attacks the parts of the brain that produce hypocretin. Emmanuel Mignot, a sleep researcher, and director of the Stanford Center for Sleep Sciences and Medicine at Stanford University explains in further detail the theory of the autoimmune history of narcolepsy. Mignot stated that a virus named Influenza A is a “trigger” that activates the response in the immune system. He also describes that Influenza A has “a small epitope of pH1N1 resembles hypocretin” (para 1). This trigger is what could possibly lead to the immune system reacting negatively to the hypocretin-producing cells. In this essay, I will discuss narcolepsy, the misconceptions that people have about the illness, health impacts, and the various pharmacological and non-pharmacological treatments.
Diseases Associated with Narcolepsy
Narcolepsy has multiple diseases called comorbid diseases. Comorbid diseases are diseases or disorders the exist along with other diseases. One main comorbid disease is cataplexy. According to Patrick, 70% of narcoleptics also struggle with cataplexy. Cataplexy is a disease that causes muscle weakness during cataplexy episodes. Some of the muscles include the face, hand, leg, and arm muscles. Some episodes can weaken all muscles in the body. When all muscles weaken at once, the sufferer may fall on the floor as if to faint. The only difference is that they remain awake and conscious the whole time (Patrick para 2). She also examined another comorbid disease, Rapid Eye Movement (REM) sleep without atonia. REM sleep is the state of sleep characterized by rapid eye movement and when dreams begin. Atony is the abrupt weakening of muscles during sleep which prevents a person from enacting their dreams. Ninety percent of all narcoleptics suffer from the absence of atonia in REM sleep (Patrick para 5). Another sleep-related condition that Patrick talked about was sleep fragmentation. This condition affects 68% of narcoleptics. Sleep fragmentation is a short halt in sleep. This condition cuts into the time narcoleptics stay asleep which can affect the quality of sleep.
There are also less common comorbid diseases are the psychiatric illnesses such as major depression which affects 2% of narcoleptics; another is a bipolar disorder which also affects 2% of narcoleptics. Anxiety disorder is another disease that affects 1% of patients.
The main reason that I took interest in this topic is because of my uncle who currently suffers from narcolepsy. This disease affected him in various detrimental ways. First, my uncle completed pharmacy school in 2010. However, he was unable to study for the qualifying exams because of his disease. Anytime he decided to study, he would suddenly fall asleep. His wife dismissed this as simply being lazy. Aside from his studies, it also affected his daily life. My uncle is the only licensed driver in his family. This means that he must drive his family everywhere. When he is behind the wheel, he begins to doze off. Normally, his wife and children must keep him awake as he drives. The serious problem is the fact that once he is alone, there is no one to keep him awake and this is when problems arise. Because of this, he has been involved in several motor vehicle accidents. Besides this, he is often unable to hold a job due to his excessive daytime sleepiness. He was constantly caught sleeping on the job, which led to his dismissal. During the night, his wife often complains that he has bouts of intense snoring followed by periods time that he stops breathing. This can even last up to a few minutes, which requires her wake her up. During these nights, he would often talk in his sleep and when his wife wakes him up, he would lie wide awake but would not move. This disease negatively impacted him and his family. I remembered that my uncle was always giving my parents excuses for avoiding family meetings, social events. My parents used to question his absence from social gatherings, and he would give an excuse that he was tired. My uncle was a Sunday school teacher at his church, and he told my parents that he felt embarrassed that the Sunday school children were making fun of that he was sleeping while teaching them.
Before the interview, I would often hear that he could not hold a job, he was involved in multiple vehicular accidents and struggled with his exams. After the interview, learning about his struggles and experiences, I began to commiserate with him. His frustration led him to seek medical attention. After being treated for his symptoms with treatments such as Continuous Positive Airway Pressure device (CPAP). The device used mainly to treat sleep apnea. And as the name suggests, it works by supplying continuous air pressure using a make and tube. Below is an image of a CPAP (Jim Hall).
Along with some medications, his quality of life improved. My uncle was able to write his exam and now working as a pharmacist in a stable hospital job. He explained to me during the interview that his life is better, and the entire family is happy for his improvement.
Common Beliefs about Narcolepsy
On the big screen, narcolepsy is often misrepresented. Based on what you might see on TV and in movies, narcolepsy is just falling to sleep at random times. According to Listal, movies like Deuce Bigalow: Male Gigolo and Scary Movie 3 have at least one character that has narcolepsy (Movies). It is often portrayed as a comical disease; this is a horrifying mistake. Below shows an image of a very common scene used in entertainment. Narcoleptics are often depicted as people that just drop to sleep in an instant, at any time.
Narcolepsy is often explained improperly by those who do not truly understand it. This leads to misunderstandings. One terrifying misunderstanding that I found is that narcolepsy isn’t serious or dangerous. This proves to be untrue. Narcolepsy is a cluster of symptoms aside from the usual daytime drowsiness. These include sleep paralysis, cataplexy, hallucinations, memory problems and many other things. These symptoms can be very dangerous to them and others around them. When episodes of cataplexy come around, the sufferer can collapse and if they are not in a safe place, injuries can occur. For narcolepsy sufferers, sleep paralysis can occur at any given time. Paralysis, along with hallucinations they can have while unable to move, can prove to be a terrifying experience.
Another misconception is that Narcoleptics collapse abruptly and frequently. Narcoleptics struggle to stay awake during the day, but there are warnings that they are about to collapse, and this gives them time to find a safe space to collapse. Through the research I conducted, I have discovered it is true that a large number of narcoleptics have episodes of muscle weakness, around “50% to 70%” according to an article I read by Collier, an experienced writer for the American Psychology Association (4). Some do fall from these brief attacks and are unable to move or speak for a period, and they do stay awake throughout this. There is also a fair amount, however, that do not experience this.
People also believe that people who sleep a lot are narcoleptic. Constantly sleeping does not prove that narcoleptics sleep more than the average person. The concern with sufferers is not the amount of sleep but, the quality of sleep. Narcolepsy sufferers are unable to get quality sleep due to interruptions caused by insomnia, night terrors, and sleep apnea. The notion that only narcoleptics sleep frequently is also wrong. Daytime drowsiness can be experienced by sufferers of sleep apnea and restless leg syndrome (Collier 6, 8). The idea that only adults can have narcolepsy is proven to be untrue according to Collier. Because of this, most children are often dismissed as lazy and do not get diagnosed until symptoms become serious and treatment becomes difficult. Approximately half of adult narcoleptics experienced signs before the age of 15. Symptoms can start as early as 7 years of age (7).
A review of evidence-based research conducted by Liblau et al. determined that the onset of narcolepsy is more prevalent around the age of 15 years while the least prevalent is around the age of 35. Refer to page 8 for example of a picture on how people mistakenly label patients who suffer from narcolepsy (320).
Story of Narcoleptics
In an article written by Karen Barrow, a journalist for the New York Times, she wrote an article that gives insight into the life of patients that live with certain with narcolepsy. Kailey Profeta, a narcolepsy sufferer, is almost completely bedridden. At the age of 9, she was diagnosed with narcolepsy. Currently, she requires medication to sleep at night, the side effect of the drugs is the nausea she experienced in the morning. During the day she must take other drugs to keep her awake. Her average life as a 16-year-old is impeded by the disease. During the third period, she has to return home to rest.
One patient that suffers from narcolepsy with cataplexy. Patricia Higgins suffered from narcolepsy in her teenage years, but it was not until her she was 32 years old that she was able to receive a proper diagnosis. Before she was diagnosed, she had to visit multiple doctors in order to find out. Narcolepsy also disturbs her life; she is a married mother of three children. She is unable, however, to work since she cannot drive. Instead, she occupies her time by volunteering with the Narcolepsy Network which is a support group for narcoleptics.
Another sufferer is Sara Kowalczyk. As a teenager, she had symptoms of cataplexy whenever she experienced strong emotions. It wasn’t until 16 that she was diagnosed with narcolepsy. When Mrs. Kowalczyk had her first child, she stopped taking her narcolepsy medication. She states that it was “scary at first but has been manageable”. The problem was that after her baby was born, she experienced worsened symptoms of narcolepsy. In her daily life, she decided to hold a job as a clinical research coordinator and study narcolepsy in college. With her understanding of the disease, she shared her knowledge and experiences with other narcoleptics.
Treatments and their Effectiveness
Medications are the most prevalent form of treatment for narcolepsy. Since there is no known cure, narcoleptics require lifetime treatment of the symptoms as they appear. In order to test the efficacy of a drug, clinical trials and studies are conducted. Some studies involve a control which is given a placebo, and an experimental group which is given the medication being tested. There are also studies where all subjects are given the drug.
One drug called Pitolisant (Wakix) was evaluated in a study by Kollb-Sielecka et al. to determine the effectiveness of the drug on narcolepsy patients with or without cataplexy. This was done with two Phase III clinical trials. The participants were placed into control and interventions groups. The participants in the control group received the placebo while the participants in the intervention group were given this drug. Pitolisant attaches itself to Histamine H3 receptors in the brain. This increases the activity of Histamine neurons which are vital for staying awake.
The results show that the clinical trial on the drug Pitolisant on patients with narcolepsy with or without cataplexy and excessive daytime sleepiness have yielded to improvements in cataplexy rates in patients. They recommended the use of the drug for patients suffering from the disease (Kollb-Sielecka et al. para 1).
Another clinical trial was used to assess the effectiveness of oral L-Carnitine in patients with narcolepsy. The study was a randomized, double-blind, cross-over and placebo-controlled trial. The results of the study show that the drug treatment greatly improved the total time of dozing off during the daytime compared to the placebo groups. (Miyagawa et al. para 1)
This study focuses on another drug used to treat narcolepsy; this drug is called sodium oxybate. The study consisted of 15 children and adolescents with narcolepsy with cataplexy all being treated with sodium oxybate. As the treatment progressed, cataplexy episodes greatly decreased as well as the severity of the episodes.
In a contrast, two of the 15 patients had to discontinue use of the drug due to constipation and dissociative feelings. Dissociative feelings being a mental process in which a person disconnects from their thoughts, feelings, or sense of identity. Another patient temporarily stopped due to body aches and dizziness but then resumed use without the symptoms reoccurring. The side effects in the four others included tremors, blurred vision, nocturnal awakenings, and increased nightmares. The side effects occurred in 6/15 of the individuals. And a positive side effect was an improvement in social/academic spheres found in 11/15 patients after beginning treatment. (Mansukhani and Shuresh para 1).
The aforementioned medications are the most common treatments; however, they only mask the symptoms of the disease. Another form of treatment is improving general nutrition such as eliminating alcohol, according to Dr. Naiman, sleep specialist at the Arizona Center for Integrative Medicine, who is quoted in Dr. Weil’s Condition Care Guide. He suggests that narcolepsy sufferers should adjust their lifestyle to assess the mental, emotional, and spiritual demands. He suggests the elimination of alcohol, caffeine, and nicotine and intake of various nutrients such as calcium, magnesium, choline, omega-3 fatty acids as well as Vitamins B, C, D and E. In addition to a change in nutritional intake, he stated that routine exercise and 15-20-minute naps will be beneficial. Dr. Naiman also advises narcoleptics need to be aware of food intolerances and their link to narcolepsy. Some of these intolerances include wheat, dairy, corn, and chocolate. He also recommends the practice of breathing exercises to manage stress and keeping a dream journal to understand and explore the psychological and spiritual impact of sleep disorders. Narcoleptics can also join a support group to receive help from individuals that have similar problems (para 13-16).
Another study conducted by Kacar et al. tested the efficacy of the combination of pharmacological with non-pharmacological intervention in childhood narcolepsy. The study conducted consisted of five patients between ages 15-16. The patients included two boys and three girls. The trial took place over a period of 33 months. Each of the patients was educated on proper nutrition, regular exercise, and proper sleep routines. Three patients were also given modafinil and the other two received methylphenidate. They, therefore, concluded that early diagnosis is vital to treat narcolepsy. They also stated that symptoms of narcolepsy greatly improved in the patients that were treated with pharmacological with non-pharmacological intervention (Kacar et al. para 1).
Conclusion
Narcolepsy is not something to laugh about. The inaccurate portrayal of narcolepsy in media has pulled a blanket of stereotypes over the eyes of the public. Overall, I have informed you of what narcolepsy is, what some of the diseases that exist with it are. I also mentioned the various treatments and stories of how people lived with narcolepsy. This paper is meant to educate you on narcolepsy and some things that we know about it.
Narcolepsy is an illness with serious consequences to the sufferers. The story of my uncle living with narcolepsy is only one story of many different stories. Narcoleptics also do not suffer from narcolepsy alone, but from a cluster of comorbid diseases that add to the struggle of daytime sleepiness, hallucination, and memory problems. Cataplexy is one of the major comorbid illnesses which adds to the problems that narcolepsy supplies. With more evidence-based research on the illness, other effective treatments will become available for the healthcare providers to utilize in treating the disease. Pharmacological treatments, such as modafinil, sodium oxybate, and pitolisant are used to treat various symptoms of narcolepsy as they appear. Non-pharmacological treatments such as nutrition, adequate sleep patterns, and exercise improve the overall quality of life for the patients.
Works Cited
Annan, Robert. “Life with Narcolepsy” Personal interview. 20 Apr. 2018.
Barrow, Karen. “Patient Voices: Narcolepsy.” The New York Times, The New York Times, 20 Mar. 2018, www.nytimes.com/interactive/2018/well/patient-voices-narcolepsy.html#pa….
Collier, Lorna. “7 Myths About Narcolepsy.” Healthgrades.com, 27 July 2017, www.healthgrades.com/conditions/7-myths-about-narcolepsy.
“Figure 3: CSF Hypocretin 1 Concentrations in People with Narcolepsy with and without Cataplexy, in Those with Idiopathic Hypersomnia, and in Controls.” Sodium Oxybate for the Treatment of Narcolepsy, narcolepsy-cataplexy-xyrem.weebly.com/pathophysiology.html.
Hall, Jim. New Sleep Apnea Treatments. 2013. https://www.heritagedentalva.com/treatments/sleep-appliances/treatment-…
Kacar, A, et al. “Efficiency of a Combination of Pharmacological Treatment and Nondrug Interventions in Childhood Narcolepsy.” Neuropediatrics., U.S. National Library of Medicine, Dec. 2016, www.ncbi.nlm.nih.gov/pubmed/27564079.
Kollb-Sielecka, Marta, et al. “The European Medicines Agency Review of Pitolisant for Treatment of Narcolepsy: Summary of the Scientific Assessment by the Committee for Medicinal Products for Human Use.” Sleep Medicine, vol. 33, May 2017, 125-129. EBSCOhost, 10.1016/j.sleep.2017.01.002.
Lee, Rachel U. and Jennifer M. Radin. “A Population-Based Epidemiologic Study of Adult-Onset Narcolepsy Incidence and Associated Risk Factors, 2004–2013.” Journal of the Neurological Sciences, vol. 370, 15 Nov. 2016, 29-34. EBSCOhost, 10.1016/j.jns.2016.08.026.
Liblau, Roland S, et al. “Hypocretin (Orexin) Biology and the Pathophysiology of Narcolepsy with Cataplexy.” Lancet Neurology, vol. 14, no. 3, Mar. 2015, 318-328. EBSCOhost, 10.1016/S1474-4422(14)70218-2.
Mansukhani, Meghna P. and Suresh Kotagal. “Sodium Oxybate in the Treatment of Childhood Narcolepsy–Cataplexy: A Retrospective Study.” Sleep Medicine, vol. 13, no. 6, June 2012, 606-610. EBSCOhost, 10.1016/j.sleep.2011.10.032.
Mignot, Emmanuel J. M. Immunologic Research, Springer US, 2014, www.ncbi.nlm.nih.gov/pmc/articles/PMC4028550/.
Miyagawa, Taku, et al. “Effects of Oral L-Carnitine Administration in Narcolepsy Patients: A Randomized, Double-Blind, Cross-Over and Placebo-Controlled Trial.” Plos ONE, vol. 8, no. 1, Jan. 2013, 1-6. EBSCOhost, 10.1371/journal.pone.0053707.
Movies > Narcolepsy Movies, www.listal.com/movies/narcolepsy.
“Narcolepsy – Dr. Weil’s Condition Care Guide.” DrWeil.com, 2 Dec. 2016, www.drweil.com/health-wellness/body-mind-spirit/sleep-issues/narcolepsy/.
Patrick, Regina. “Narcolepsy with Comorbid Conditions.” Sleep Review, www.sleepreviewmag.com/2015/05/narcolepsy-comorbid-conditions/.